Unfortunately, the very places we go to receive health care put us at risk for becoming infected with superbugs, bacteria exposed to so many antibiotics that they have become immune to their effects. Clostridium difficile (C. diff) is one such bacteria. It causes inflammation of the colon and rampant diarrhea that can have life-threatening consequences. Part of its virulence lies in the tough spores formed by the bacteria. They are responsible for starting infections in the colon and for spreading the disease. New research has provided insight into what triggers the spores to infect.
A discovery by a research team from the University of Michigan Medical School and the US Food and Drug Administration (FDA) found that for C. diff spores to germinate and cause infection, they need calcium in the gut.
The research study and findings by senior author Philip C. Hanna at the University of Michigan and colleagues were published July 13 in the online journal PLoS Pathogens.
The Problem with C Diff
Clostridium difficileinfects a half million people and causes 15,000 deaths in the US each year. Most C. diff infections happen in the hospitals, where already sick people inadvertently ingestC. diff bacteria from contact with people or equipment contaminated with it. The infection causes severe diarrhea, inflammation, and death of cells lining the intestines from the toxins released by the bacteria.
Replacement of fluids lost through diarrhea and treatment with vancomycin or fidaxomicin antibiotics are the usual treatments for C. diff. The FDA has not approved metronidazole for treating C. diff infections, but doctors sometimes recommend it for mild cases. However, treatment is complicated by the facts that the organism is rapidly becoming resistant to the drugs used to treat it and in 20% or more of the cases, the infection recurs, making effective treatment even harder. The Centers for Disease Control and Prevention have put it in the Urgent Threat to global health category because of the number of deaths it causes and the estimated 4 billion healthcare dollars C. diff care is projected to cost in the next five years.
Fecal transplants — either by placement of live fecal bacteria from a healthy donor into the gastrointestinal tract or oral ingestion of dehydrated stool in capsule form — have shown high infection cure rates. Recent studies on C. diff patients who had a fecal transplant showed that beneficial types of healthy bacteria their can persist for years.

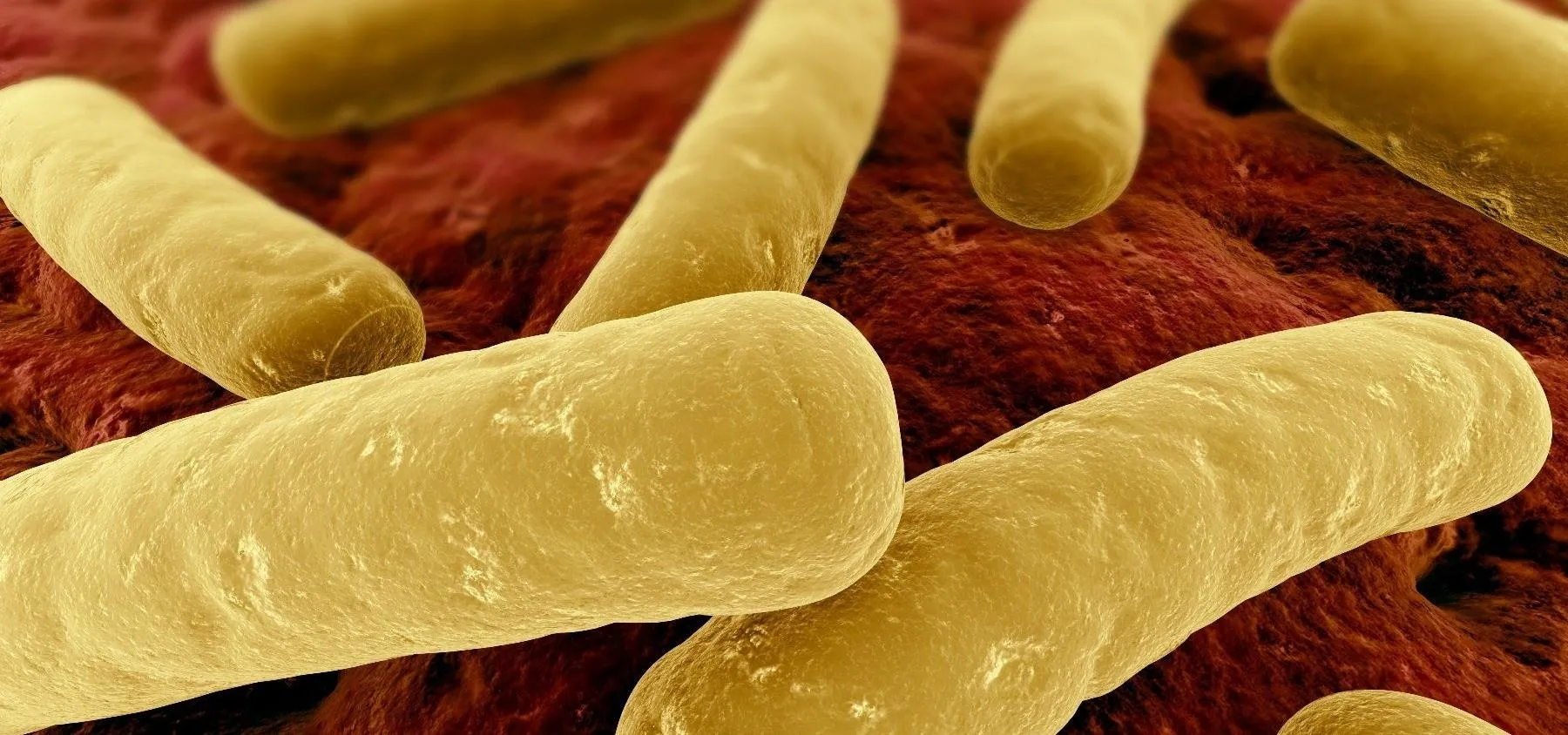
Clostridium difficile bacteria cells in the process of forming hard-shelled spores. The small bright particles are spores, while the long dark rod-shapes are C. diff bacteria cells.
The release of toxins is what causes the symptoms of C. diff, but the infection itself depends on the production of spores. Spores ensure that the bacteria, which is exquisitely sensitive to oxygen, keeps itself alive in a form where it can survive the presence of oxygen.
The bacteria form spores that are survive through heat, radiation, antibiotics, and chemicals, including alcohol-based hand cleansers and conventional surface cleaners. This toughness keeps the spores alive and available for someone to pick up through contact. With just a little hand-to-mouth action, the spores are ingested. The spores are also acid-resistant, and that allows them to pass through the stomach unharmed. Once the spores make their way to the gut and get exposed to bile acids and glycine, they germinate and multiply into bacterial cells in the colon, setting off the infection.
One way to stop a C. diff infection is to prevent it in the first place. By disabling the ability of the spores to germinate, it's possible that could stop an infection from getting a stronghold in the gut. Research by Hanna and his colleagues have identified a key component C. diff spores need to germinate.
How Calcium Sets Off an Infection
A keen observation by Hanna's graduate student Travis Kochan led the research team to pursue the role of calcium in spore germination. Kochan noticed that the liquid culture media used to grow C. diff has calcium in it. He made a culture medium without calcium and found no spores germinated in that medium.
When the researchers mutated the spores so that they didn't need glycine to germinate, the spores were able to germinate in mice given calcium. They learned that glycine could release calcium from the spore core, but that if extra calcium was already present — like from taking medications that contain calcium — glycine wasn't needed for germination.
The authors believe their findings help explain why some hospital patients and nursing home residents have a much higher risk of being infected with C. diff. These are groups of people who often have extra calcium in their guts from medication or supplements at the hospital. Hanna cautions that patients should not stop taking their medications or doctor-recommended supplements based on his research. His studies were in mice, and more studies are needed to confirm them in humans before making any recommendations regarding calcium.
These spores are like armored seeds, and they can pass through the gut's acidic environment intact. Much of the spore's own weight is made of calcium, but we've shown that calcium from the gut can work with bile salts to trigger the enzyme needed to activate the spore and start the germination process.
The first step in figuring out how to stop a process is to learn what makes it run. The research team has just added to our knowledge of what makes C. diff spores germinate to set up an infection. The study authors suggest that restricting calcium in the intestine of at-risk patients — like those in healthcare settings — holds the potential to prevent Clostridium difficile infections.
- Follow Invisiverse on Facebook and Twitter
- Follow WonderHowTo on Facebook, Twitter, Pinterest, and Google+
Cover image via Tim Sandle/Flickr



Comments
No Comments Exist
Be the first, drop a comment!